Sweating is a natural process that helps regulate body temperature, but for some people, it goes into overdrive. Hyperhidrosis, or excessive sweating, affects about 1-5% of the population and can significantly impact quality of life, causing discomfort, embarrassment, and even social withdrawal. Fortunately, there are several evidence-based treatments available, ranging from simple over-the-counter options to advanced medical procedures. Let’s break them down in an easy-to-read guide, backed by science.
What Is Hyperhidrosis?
Hyperhidrosis is a condition where the body produces sweat beyond what’s needed for temperature control. It’s often categorized into two types:
- Primary hyperhidrosis: Typically affects specific areas like the armpits, hands, feet, or face, and is thought to stem from overactive sweat glands, possibly due to genetics or nerve signaling issues.
- Secondary hyperhidrosis: Caused by an underlying condition (e.g., diabetes, menopause, or medication side effects) and tends to be more widespread.
Since treatments vary depending on the type and severity, it’s worth seeing a doctor to pinpoint the cause. Now, let’s explore the options.
1. Antiperspirants: The First Line of Defense
For many, the journey starts with antiperspirants—not the regular drugstore kind, but clinical-strength versions with aluminum chloride (usually 10-20%). These work by plugging sweat ducts, reducing how much sweat reaches the skin’s surface.
- How to Use: Apply to dry skin at night (when sweat glands are less active) and wash off in the morning. Start with 2-3 times a week.
- Effectiveness: Studies have found that aluminum chloride antiperspirants reduced sweating by 30-70% in people with mild-to-moderate axillary (armpit) hyperhidrosis.
- Pros: Cheap, easy to find (brands like Carpe or SweatBlock), non-invasive.
- Cons: Can irritate sensitive skin; less effective for severe cases or areas like hands and feet.

2. Medications: Pills and Patches to Calm the Sweat
When antiperspirants don’t cut it, oral or topical medications might help. These target the nervous system, which controls sweating.
- Oral anticholinergics (e.g., glycopyrrolate, oxybutynin): These block the nerve signals that trigger sweat glands.
- Evidence: Multiple studies have demonstrated significant generalized improvement in sweating with oral cholinergic medicatinos.
- Pros: Works for widespread sweating.
- Cons: Side effects like dry mouth, constipation, or blurry vision can be a dealbreaker for some.
- Topical Glycopyrrolate: A wipe applied to affected areas (e.g., Qbrexza).
- Evidence: Approved by the FDA in 2018, clinical trials showed a 60% reduction in armpit sweating after 4 weeks.
- Pros: Fewer systemic side effects than pills.
- Cons: Prescription-only and pricey without insurance. That being said, visit their website to see if your applicable for their savings cards. Many patients pay very little to nothing with commercial insurance.
3. Iontophoresis: A Gentle Electric Solution
This treatment uses a device that sends a mild electric current through water-soaked skin (usually hands or feet) to “stun” sweat glands into producing less.
- How It Works: You soak your hands or feet in trays of water for 20-30 minutes, 2-3 times a week.
- Evidence: A 2017 study reported up to 93% sweat reduction after 2 weeks in patients with palmar (hand) hyperhidrosis.
- Pros: Non-invasive, drug-free, and safe for long-term use.
- Cons: Time-consuming; devices cost $100-$500 upfront; less effective for armpits. Be sure to navigate options for devices with your physician.
4. Botox: Freezing Sweat Glands in Their Tracks
Botulinum toxin (Botox) injections are a game-changer for severe, localized hyperhidrosis. They block the nerve signals that tell sweat glands to activate.
- How It Works: A doctor injects small amounts into the affected area (e.g., 50-100 units per armpit). Effects kick in within a week and last 4-12 months.
- Evidence: Multiple studies have demonstrated the efficacy of Botulinum toxin for hyperhidrosis. One landmark study by Heckmann et al in the NEJM quantified the degree of improvement down to the mg of sweat/minute. Even 2 months after treatment patients had a marked improvement in sweating with 98% recommending this therapy to others.
- Pros: Highly effective, FDA-approved since 2004, quick procedure.
- Cons: Temporary stinging during injections; not ideal for large areas.
Botox is an incredible treatment for axillary hyperhidrosis. Read everything about this procedure here!
5. Microwave Therapy: A High-Tech Zap
Known as miraDry, this FDA-approved device uses microwave energy to permanently destroy sweat glands in the armpits.
- How It Works: A handheld device heats and eliminates sweat glands in a 60-minute outpatient session.
- Evidence: A 2012 study showed that 90% had at least a 50% reduction in baseline sweating, with a significant improvement in quality of life!
- Pros: Long-lasting; also reduces underarm odor and hair.
- Cons: Costly ($1,500-$3,000); only for armpits; possible temporary swelling or numbness.
Find a provider with Microwave therapy by visiting this site!
6. Surgery: The Last Resort
For extreme cases that don’t respond to other treatments, surgical options like endoscopic thoracic sympathectomy (ETS) might be considered.
- How It Works: Surgeons cut or clamp nerves in the chest that trigger sweating in the hands or face.
- Evidence: Multiple studies have corroborated the long-term benefits of ETS, citing long-term sweat reduction and patient satisfaction.
- Pros: Permanent relief for hands or face.
- Cons: Invasive; risk of side effects like compensatory sweating or nerve damage.
ETS has been shown to be more effective/satisfactory for younger patients and for those with hyperhidrosis of the palms. It is important to find a reputable neurosurgeon near you that has performed many of these surgeries.
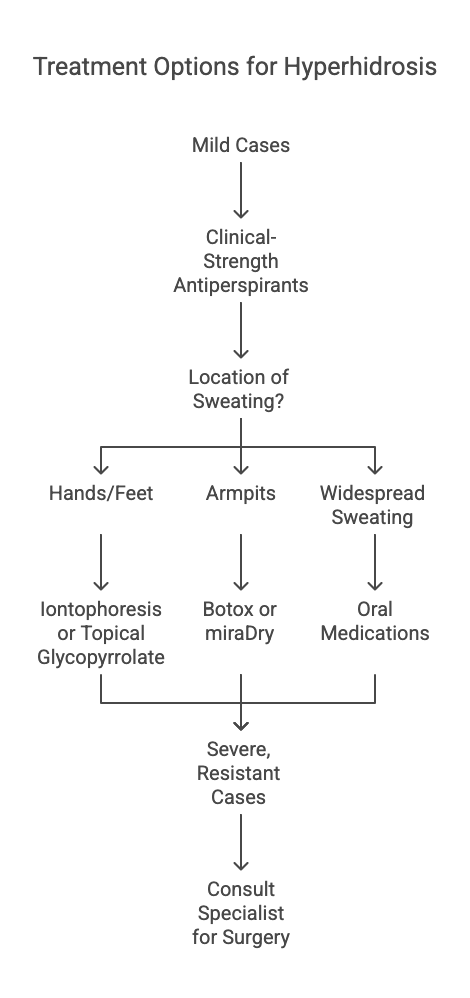
Which Treatment Is Right for You?
- Mild cases: Start with clinical-strength antiperspirants.
- Hands/Feet: Try iontophoresis or topical glycopyrrolate.
- Armpits: Botox or miraDry are top picks.
- Widespread sweating: Oral meds might be the answer.
- Severe, resistant cases: Talk to a specialist about surgery.
Always consult a dermatologist to tailor the approach to your needs. Hyperhidrosis doesn’t have a one-size-fits-all cure, but with these options, relief is within reach.
Additional Sources
- Pariser, D. M., et al. (2014). Dermatol Clin 32 (2014) 485–490, http://dx.doi.org/10.1016/j.det.2014.06.008
- Cleveland Clinic. “Hyperhidrosis (Excessive Sweating): Diagnosis & Treatment.” https://my.clevelandclinic.org/health/diseases/16927-hyperhidrosis
- U.S. Food & Drug Administration. “Qbrexza (glycopyrronium) topical wipes, for topical use.” https://www.accessdata.fda.gov/drugsatfda_docs/label/2018/209259s000lbl.pdf
- International Hyperhidrosis Society. “Iontophoresis for excessive sweating.” https://www.sweathelp.org/hyperhidrosis-treatments/iontophoresis.html
- Mayo Clinic. “Hyperhidrosis – Diagnosis and treatment.” https://www.mayoclinic.org/diseases-conditions/hyperhidrosis/diagnosis-treatment/drc-20367169
- American Academy of Dermatology. “Hyperhidrosis: Diagnosis and Treatment.” https://www.aad.org/public/diseases/a-z/hyperhidrosis-treatment
- miraDry. “miraDry® Clinical Studies.” https://www.miradry.com/miradry-clinical-studies/
- Doolittle, J., et al. “Hyperhidrosis: an update on prevalence, impact, and management.” Annals of the New York Academy of Sciences, vol. 1313, no. 1, 2014, pp. 13-25. https://nyaspubs.onlinelibrary.wiley.com/doi/full/10.1111/nyas.12407

Leave a comment