Oral medications play a crucial role in managing hidradenitis suppurativa (HS), particularly for moderate to severe cases, or when topical treatments alone are insufficient. These medications work systemically, targeting inflammation and other underlying disease processes throughout the body.
Categories of Oral Medications Used in HS
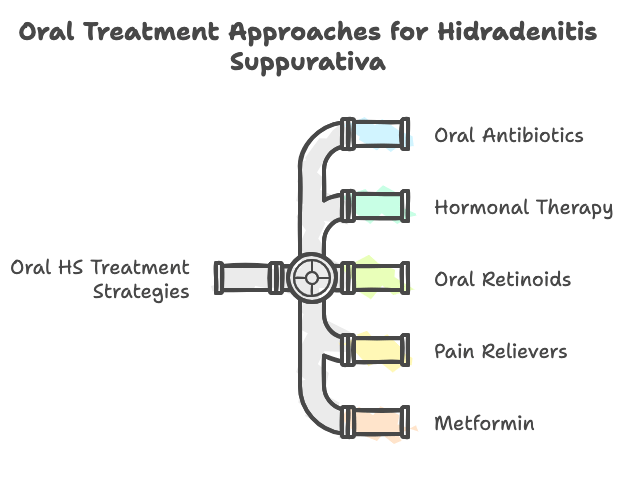
- Oral Antibiotics: Antibiotics, such as doxycycline, clindamycin, and rifampin, are frequently used in HS treatment. While HS is not primarily a bacterial infection, these antibiotics possess anti-inflammatory properties that help to reduce lesion severity and flare-ups. Combination therapy with clindamycin and rifampin has shown particular efficacy in some studies. Long-term, low-dose antibiotic use may be considered for some patients to maintain disease control, but concerns about antibiotic resistance and side effects need to be carefully weighed.
- Hormonal Therapy: Hormonal therapies can be beneficial for women with HS, especially those who experience flares related to their menstrual cycle. Estrogen-containing contraceptives and spironolactone are sometimes prescribed to regulate hormone levels and reduce inflammation. Spironolactone, an anti-androgen medication, can be particularly helpful in women with hormonal imbalances contributing to their HS. Hormonal therapy is often used in combination with other treatments.
- Oral Retinoids: Retinoids like isotretinoin and acitretin, vitamin A derivatives, are used to normalize epithelial cell function and reduce inflammation in various skin conditions. While oral retinoids are not considered first-line treatments for HS, they may be helpful in some patients, particularly those with inflammatory flares or associated acne-like lesions. However, their effectiveness in HS is variable, and they are often used in combination with other therapies. Due to potential side effects, including teratogenicity (risk of birth defects), retinoids require careful monitoring and are contraindicated in pregnancy.
- Pain Relievers: Pain management is a critical aspect of HS care. Non-steroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen or naproxen, can help manage mild to moderate pain associated with HS lesions. For more severe pain, opioids may be considered, but their use is generally limited to short-term management of acute flares due to the risk of dependence and other side effects. Non-opioid pain management strategies are increasingly emphasized in chronic HS pain.
- Metformin: Metformin, a medication primarily used for type 2 diabetes, has shown promise in HS treatment. It is thought to improve insulin sensitivity and possess anti-inflammatory properties that may be beneficial in HS. Metformin may be particularly helpful in patients with HS who also have metabolic syndrome or insulin resistance, common comorbidities of HS. Studies suggest metformin can reduce HS lesion severity and improve patient-reported outcomes.
Biologic Medications: Targeted Immunotherapy
Biologics represent a significant advancement in the treatment of moderate to severe HS that has not responded adequately to conventional therapies. These medications are targeted immunotherapies that specifically block key inflammatory molecules involved in HS pathogenesis. Currently approved and investigational biologics for HS include:
Biologics are a significant advancement for moderate to severe HS, targeting specific inflammatory molecules. Approved and investigational biologics include:
- Adalimumab (Humira): Targets TNF-α to reduce inflammation and is approved for HS treatment.
- Infliximab (Remicade): Another TNF-α inhibitor, also effective in reducing inflammation in HS.
- Secukinumab (Cosentyx): Targets IL-17A to disrupt the inflammatory process and is approved for HS.
- Bimekizumab-bkzx (Bimzelx): Dual IL-17A and IL-17F inhibitor, approved for HS, offering a more comprehensive disruption of IL-17 pathways.
Therapeutic drug monitoring is often employed to optimize biologic treatment by assessing drug levels and identifying potential treatment failures.
Conclusion:
HS remains a stubborn and challenging condition to treat. Recently multiple sophisticated and efficacious treatments have been FDA approved, with many more pending late stage trials. It is wonderful that our patients have more options when it comes to navigating this often debilitating condition.
Note* Even with these aforementioned medical advances, patients may have recurrent, persistent areas that do not resolve. In that case, surgical options should be explored.
References
Hidradenitis suppurativa – Diagnosis and treatment – Mayo Clinic, accessed February 8, 2025, https://www.mayoclinic.org/diseases-conditions/hidradenitis-suppurativa/diagnosis-treatment/drc-20352311
A concise clinician’s guide to therapy for hidradenitis suppurativa – PMC, accessed February 8, 2025, https://pmc.ncbi.nlm.nih.gov/articles/PMC7105662/
Guide to Biologics for Hidradenitis Suppurativa – Everyday Health, accessed February 8, 2025, https://www.everydayhealth.com/hidradenitis-suppurativa/consumers-guide-to-biologics/
Hidradenitis Suppurativa: Advancing Treatment With Biologics, accessed February 8, 2025, https://www.ajmc.com/view/hidradenitis-suppurativa-advancing-treatment-with-biologics
Systemic clindamycin plus rifampicin therapy for hidradenitis suppurativa: A systematic review and meta-analysis – PubMed, accessed February 10, 2025, https://pubmed.ncbi.nlm.nih.gov/33831285/
Systemic retinoids for hidradenitis suppurativa: A systematic review and meta-analysis – PubMed, accessed February 10, 2025, https://pubmed.ncbi.nlm.nih.gov
Metformin for hidradenitis suppurativa, https://pubmed.ncbi.nlm.nih.gov
Hidradenitis Suppurativa Treatments – UMass Chan Medical School, accessed February 8, 2025, https://www.umassmed.edu/hs-center/treatments/
Hidradenitis suppurativa (HS) & other conditions (comorbidities) – No BS About HS, accessed February 8, 2025, https://www.nobsabouths.com/what-is-hidradenitis-suppurativa/other-conditions

Leave a comment