Introduction
Heat shock proteins (HSPs) are a family of highly conserved proteins that act as molecular chaperones, crucial for maintaining cellular homeostasis. They play a vital role in protein folding, preventing protein aggregation, and facilitating the repair of damaged proteins under various cellular stresses. This article will explore the primary literature evidence demonstrating how lifestyle interventions such as diet, exercise, and heat therapy can modulate HSP expression and function. Furthermore, we will examine the connection between HSPs and metabolic disease, and their complex relationship with cancer, including potential therapeutic strategies.
Stimulating Heat Shock Proteins Through Lifestyle Interventions
Dietary Strategies
Polyphenols: Polyphenols, bioactive compounds found in various plant-based foods, have demonstrated the ability to modulate HSP expression. Tea polyphenols, extracted from tea leaves, have been shown in in vivo and in vitro heat stress models to enhance antioxidant capacity and induce HSPs, thereby relieving heat stress injury in myocardial cells. Specifically, tea polyphenol supplementation at 10 μg/mL effectively relieved heat damage in H9C2 cells at 42°C, showing reduced cellular degeneration. This suggests that dietary intake of polyphenol-rich foods could be a viable strategy to enhance HSP expression and cellular resilience.
Calorie Restriction: Caloric restriction (CR), a dietary regimen characterized by reduced calorie intake without malnutrition, has been linked to increased HSP expression. A study on rats demonstrated that both acute (48-hour fasting) and chronic CR significantly increased hsp70 mRNA levels in the stomach and duodenum. This upregulation of HSP70, a key cytoprotective HSP, in the gut suggests a potential mechanism by which CR may exert its beneficial effects, possibly contributing to longevity and delayed onset of age-related diseases.
High-Fat Diet: While some studies indicate that high-fat diets can reduce HSP expression in certain tissues like muscle , other research suggests a more nuanced relationship. Interestingly, short-term high-fat feeding in animal models has shown no significant reduction in skeletal muscle HSP72 expression and may even lead to an initial increase, potentially as a compensatory response to metabolic dysfunction. However, long-term high-fat feeding appears to result in a significant decrease in HSP72 expression, similar to observations in type 2 diabetes. This complex interplay indicates that while short-term metabolic stress might induce a protective HSP response, chronic metabolic stress associated with sustained high-fat diets may ultimately impair HSP expression and function. More research is needed to fully elucidate the long-term effects of different dietary fat compositions and durations on HSP expression in various tissues and metabolic contexts.
Exercise
Exercise, a potent physiological stressor, is a well-established stimulus for HSP induction. Studies have shown that various forms of exercise can upregulate HSPs:
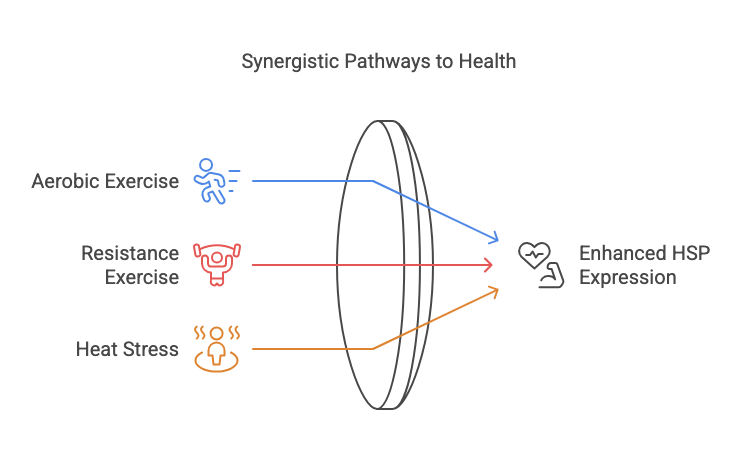
- Aerobic Exercise: Prolonged aerobic exercise has been shown to induce the release of HSP72 from the human brain in vivo. In a study examining cerebral HSP72 release during exercise, a significant increase in HSP72 release from the brain was observed after 180 minutes of moderate exercise. This finding suggests that exercise-induced stress can trigger HSP release from the brain, potentially playing a role in neuroprotection and stress adaptation.
- Resistance Exercise and Heat Stress: Combining resistance exercise with whole-body heat stress further enhances HSP expression. Research on resistance-trained individuals demonstrated that resistance exercise followed by heat stress significantly increased the expression of HSPA and activation of the Akt-mTOR cascade in skeletal muscle, compared to resistance exercise alone. This synergistic effect suggests that combining exercise with heat exposure could be a particularly effective strategy to maximize HSP induction in muscle tissue.
Exercise-induced HSP upregulation is complex and influenced by exercise type, intensity, and duration. While acute exercise leads to transient increases in HSP expression, chronic training may result in minimal elevations post-exercise due to adaptation. However, exercise training consistently demonstrates an overall increase in basal HSP levels over time.
Heat Therapy/Sauna
Passive heat therapy, such as sauna bathing, is a direct method to induce the heat shock response and stimulate HSP production. Studies using Finnish saunas have demonstrated that even a single sauna session can significantly increase serum HSP70 levels in both trained and untrained men. One study observed a 144% and 271% increase in serum HSP70 after the first sauna session in trained and untrained individuals, respectively. Repeated sauna sessions, while still increasing HSP70, may elicit a smaller relative increase compared to the initial session, indicating an adaptive response to repeated heat stress.
Furthermore, heat therapy has been shown to elevate extracellular HSP70 (eHSP70) levels, similar to exercise. A study comparing exercise and passive heating via warm water immersion found that both interventions elevated eHSP70, although exercise induced a larger magnitude of change. This suggests that while exercise may be a more potent stimulus, passive heating offers a feasible alternative for individuals unable to engage in regular exercise to induce HSPs and potentially gain associated health benefits.
Heat Shock Proteins and Metabolic Disease
Emerging evidence highlights a crucial role for HSPs in metabolic health and disease. Reduced HSP72 expression has been observed in the skeletal muscle of individuals with type 2 diabetes and insulin resistance. Conversely, studies in rodents have shown that heat treatment, transgenic overexpression, or pharmacological induction of HSP72 can prevent high-fat diet-induced glucose intolerance and skeletal muscle insulin resistance. This inverse relationship suggests that HSPs, particularly HSP72, play a protective role against metabolic dysfunction.
The connection between HSPs and metabolic disease may be related to HSPs’ role in regulating insulin sensitivity and glucose homeostasis. Heat treatments have been shown to improve whole-body glucose homeostasis and insulin-stimulated glucose uptake in skeletal muscle, alongside increased HSP72 expression. This suggests that HSP induction may contribute to improved insulin signaling and glucose metabolism, potentially mitigating the development of metabolic diseases like type 2 diabetes. Further research is needed to fully elucidate the molecular mechanisms by which HSPs influence metabolic pathways and insulin sensitivity.
Heat Shock Proteins and Cancer: A Complex Relationship and Therapeutic Targets
In the context of cancer, HSPs exhibit a complex, often paradoxical, “double-edged sword” role. While HSPs are essential for cellular survival and stress adaptation, they are frequently overexpressed in various cancers and implicated in tumor progression, metastasis, and resistance to therapy.
- Pro-tumorigenic Roles: Elevated HSP levels in cancer cells can promote cell proliferation, inhibit apoptosis, and enhance tumor cell survival under stressful tumor microenvironments and during anticancer therapies. Specific HSPs, such as HSP27, HSP70, and HSP90, have been associated with poor prognosis in various cancers and chemoresistance. For example, HSP27 overexpression is linked to chemoresistance in lung cancer stem cells, while HSP70 and HSP27 are implicated in chemotherapy resistance in breast cancer.
- Therapeutic Targets: Despite their pro-tumorigenic roles, HSPs are also being explored as therapeutic targets in cancer. The dependence of cancer cells on HSPs for survival and stress adaptation creates a vulnerability that can be exploited. Strategies targeting HSPs in cancer therapy include:
- Pharmacological Inhibition: Inhibitors of HSP90, in particular, have been extensively studied and tested in clinical trials. HSP90 inhibitors can disrupt the chaperone function of HSP90, leading to the degradation of numerous oncogenic client proteins and triggering antitumor effects.
- HSP-based Cancer Vaccines: HSPs can bind to tumor-associated antigens, forming complexes that can be recognized by antigen-presenting cells, stimulating antitumor immune responses. This property is being explored for the development of HSP-based cancer vaccines to enhance immune recognition and destruction of cancer cells.
The dual nature of HSPs in cancer necessitates a nuanced therapeutic approach. While HSP inhibition holds promise for disrupting cancer cell survival and overcoming therapy resistance, strategies to selectively modulate HSP function in tumor versus normal cells are crucial to minimize potential toxicity and maximize therapeutic efficacy.
Conclusion
Primary literature provides compelling evidence that lifestyle interventions such as dietary modifications (polyphenol-rich diets, calorie restriction), regular exercise, and heat therapy/sauna can effectively stimulate heat shock protein expression and potentially enhance their function. These interventions induce cellular stress responses that trigger the upregulation of these protective chaperones. Furthermore, dysregulation of HSPs is implicated in metabolic diseases and cancer, highlighting their critical role in health and disease. While HSPs play complex and sometimes opposing roles in cancer, targeting HSPs represents a promising avenue for novel therapeutic strategies. Future research should continue to explore the precise mechanisms by which lifestyle factors and therapeutic interventions modulate HSP function and their impact on various physiological processes and disease states.
Sources:
- Tea Polyphenols Enhanced the Antioxidant Capacity and Induced Hsps to Relieve Heat Stress Injury: https://pmc.ncbi.nlm.nih.gov/articles/PMC8369192/
- Caloric restriction increases the expression of heat shock protein in the gut: https://pubmed.ncbi.nlm.nih.gov/8651750/
- Exercise, heat shock proteins and insulin resistance: https://royalsocietypublishing.org/doi/10.1098/rstb.2016.0529
- Effect of heat stress on heat shock protein expression and hypertrophy-related signaling in the skeletal muscle of trained individuals: https://journals.physiology.org/doi/full/10.1152/ajpregu.00031.2023
- Exercise induces the release of heat shock protein 72 from the human brain in vivo: https://pmc.ncbi.nlm.nih.gov/articles/PMC1065286/
- The effects of a single and a series of Finnish sauna sessions on the immune response and HSP-70 levels in trained and untrained men: https://www.tandfonline.com/doi/full/10.1080/02656736.2023.2179672
- The effect of passive heating on heat shock protein 70 and interleukin-6: A possible treatment tool for metabolic diseases?: https://pmc.ncbi.nlm.nih.gov/articles/PMC5605168/
- Heat shock proteins: Biological functions, pathological roles, and therapeutic opportunities: https://pmc.ncbi.nlm.nih.gov/articles/PMC9345296/
- Heat Shock Proteins, a Double-Edged Sword: Significance in Cancer Progression, Chemotherapy Resistance and Novel Therapeutic Perspectives: https://www.mdpi.com/2072-6694/16/8/1500
- Heat shock proteins in cancer: diagnostic, prognostic, predictive, and treatment implications: https://pmc.ncbi.nlm.nih.gov/articles/PMC1176476/
- Targeting Heat Shock Proteins in Cancer: A Promising Therapeutic Approach: https://www.mdpi.com/1422-0067/18/9/1978
- Intracellular and extracellular functions of heat shock proteins: repercussions in cancer therapy: https://academic.oup.com/jleukbio/article/81/1/15/6975862

Leave a comment