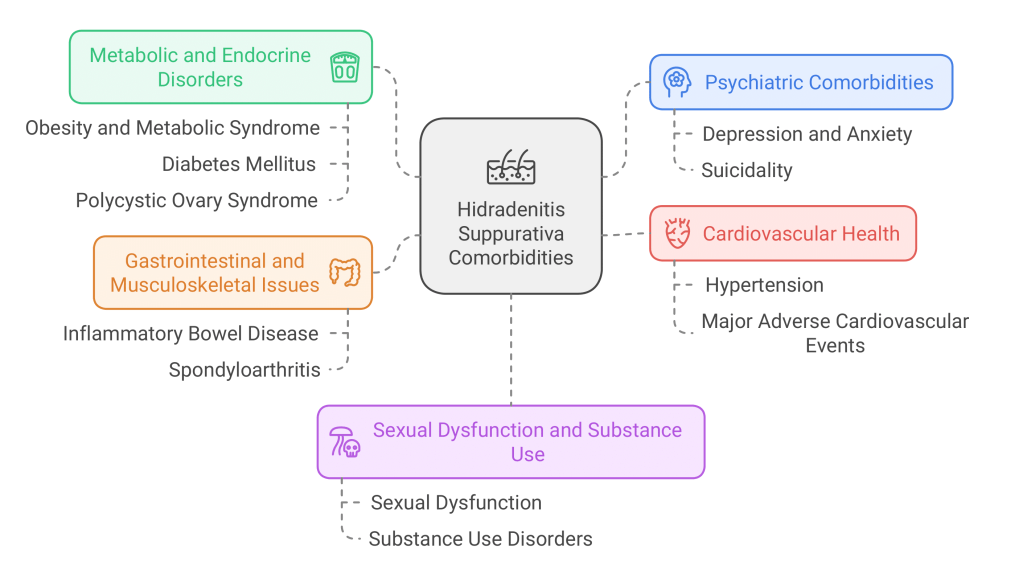
Hidradenitis suppurativa (HS), a chronic inflammatory skin disorder, has a high comorbidity burden that extends far beyond its painful physical manifestations. This comprehensive study, developed by the U.S. and Canadian Hidradenitis Suppurativa Foundations, provides evidence-based screening recommendations for the wide range of comorbidities associated with HS, including metabolic, psychiatric, and cardiovascular diseases.
Study Overview and Methodology
The research involved systematic reviews and meta-analyses to assess the prevalence and incidence of over 30 comorbid conditions in HS patients, comparing them to control groups from the general population. Using these data, the researchers formulated screening recommendations based on the prevalence and strength of association of each condition with HS.
Key Findings
1. Psychiatric Comorbidities
- Depression and Anxiety: HS patients are at higher risk for both depression and generalized anxiety disorder, with depression rates as high as 26%. Screening for these conditions is recommended, especially for patients exhibiting signs of psychological distress.
- Suicidality: Evidence from European studies indicates that HS patients have a higher incidence of completed suicide, underscoring the importance of mental health support in this population.
2. Metabolic and Endocrine Disorders
- Obesity and Metabolic Syndrome (MetS): HS patients exhibit a three-fold increase in obesity prevalence, while MetS affects 10.4% to 50.6% of this population. Regular screening for these conditions, given their influence on HS severity, is recommended.
- Diabetes Mellitus (DM): The risk of DM is elevated in HS patients, with prevalences reaching up to 24.8%. Screening for diabetes is crucial for comprehensive HS management.
- Polycystic Ovary Syndrome (PCOS): Among female HS patients, the prevalence of PCOS is notably high, necessitating endocrine evaluation to manage this coexistent condition.
3. Cardiovascular Health
- Hypertension: HS patients face a higher risk of hypertension, which is influenced by related factors like obesity and smoking. Regular blood pressure monitoring is advised.
- Major Adverse Cardiovascular Events (MACE): Chronic systemic inflammation in HS may contribute to cardiovascular events, making early detection and lifestyle intervention essential for reducing risks.
4. Gastrointestinal and Musculoskeletal Issues
- Inflammatory Bowel Disease (IBD): Crohn’s disease and ulcerative colitis are more common in HS patients. Given their shared inflammatory pathways, screening for IBD can lead to earlier intervention and better overall patient outcomes.
- Spondyloarthritis: The prevalence of spondyloarthropathies in HS patients supports the need for regular screening for joint and musculoskeletal symptoms.
5. Sexual Dysfunction and Substance Use
- Sexual Dysfunction: The prevalence of sexual dysfunction in HS patients underscores the need for addressing sexual health, particularly given the involvement of HS in areas impacting sexual function.
- Substance Use Disorders: Smoking and opioid use disorders are more prevalent among HS patients. These findings support the need for substance use screening and cessation interventions as part of holistic HS care.
Clinical Implications
The study concludes that dermatologists and primary care providers should routinely screen HS patients for a variety of comorbidities, including obesity, diabetes, hypertension, and mental health disorders. Such screenings could improve long-term health outcomes and reduce the overall morbidity associated with HS. By incorporating these screenings into standard care practices, healthcare providers can help mitigate the far-reaching impacts of this condition.

Leave a comment