The United States healthcare system is often lauded for its advancements in medical technology and treatment options. However, beneath the surface lies a complex web of administrative hurdles that can impede patient care and contribute to physician burnout. Central to these issues are Pharmacy Benefit Managers (PBMs), insurance formularies, and prior authorizations. While these mechanisms were initially designed to control costs and ensure appropriate use of medications, they have evolved in ways that often negatively impact patients and healthcare providers. This article delves deep into how these systems function, the evidence-backed repercussions they have on patient outcomes and physician well-being, and explores alternative solutions and advocacy pathways for meaningful reform.
Understanding Pharmacy Benefit Managers (PBMs)
Who Are PBMs and What Do They Do?
PBMs are third-party intermediaries that manage prescription drug benefits on behalf of health insurers, Medicare Part D drug plans, large employers, and other payers. They are responsible for:
- Negotiating with Drug Manufacturers: PBMs secure rebates and discounts from pharmaceutical companies in exchange for favorable placement on formularies.
- Contracting with Pharmacies: They establish reimbursement rates for pharmacies dispensing medications.
- Formulary Management: PBMs decide which drugs are covered under an insurance plan and at what tier.
The Lack of Transparency and Its Consequences
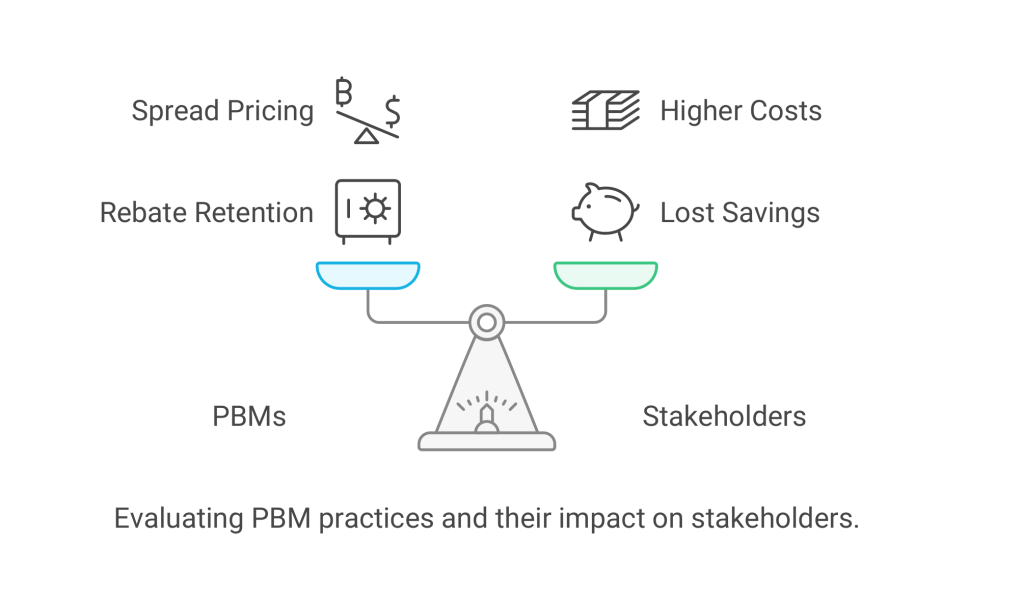
Despite their role in managing drug benefits, PBMs often operate with little transparency:
- Rebate Retention: PBMs may keep a significant portion of rebates from drug manufacturers instead of passing savings to insurers or patients.
- Spread Pricing: They may charge insurers more for a drug than they reimburse the pharmacy, pocketing the difference.
A report by the Senate Finance Committee revealed that PBMs retain up to 50% of the rebates provided by drug manufacturers1. This practice can inflate drug prices and increase costs for patients.
Insurance Formularies and Prior Authorizations
The Structure and Impact of Insurance Formularies
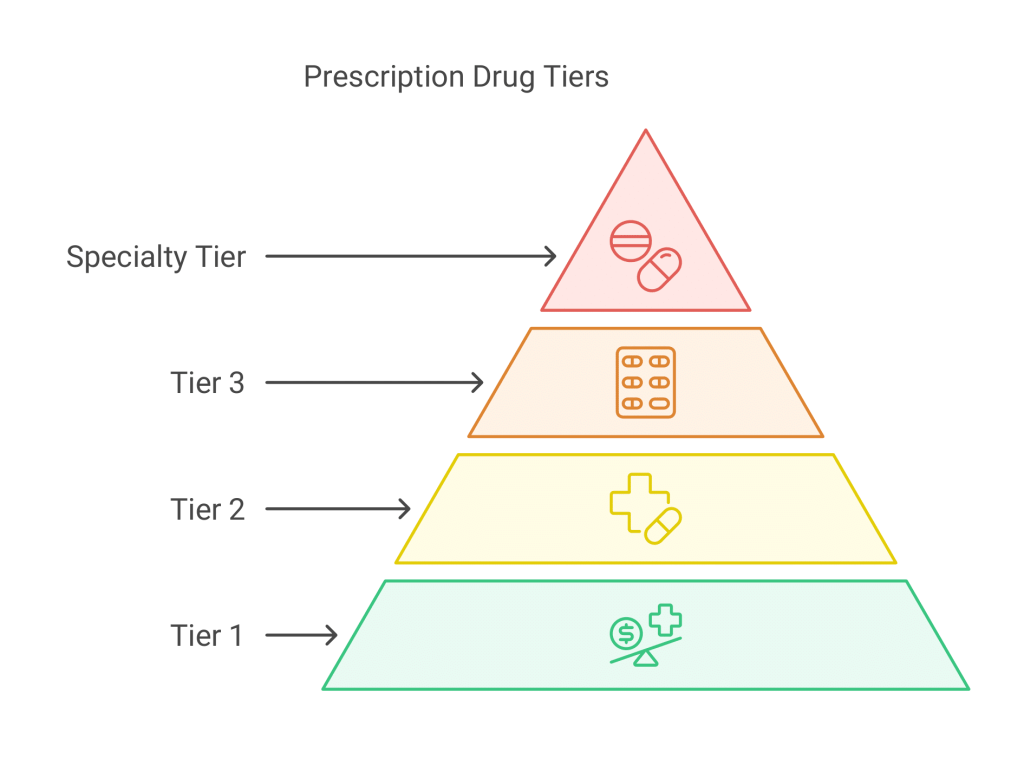
An insurance formulary is a list of medications that an insurance plan covers, often organized into tiers that determine patient cost-sharing:
- Tier 1: Generic drugs with the lowest co-pays.
- Tier 2: Preferred brand-name drugs with moderate co-pays.
- Tier 3: Non-preferred brand-name drugs with higher co-pays.
- Tier 4/Specialty Tier: High-cost medications with the highest co-pays or co-insurance.
Impact on Patients:
- Limited Access: Medications not on the formulary may not be covered, forcing patients to pay out-of-pocket or forego treatment.
- Higher Costs: Placement of drugs in higher tiers increases patient expenses.
The Burden of Prior Authorizations
Prior authorization is a requirement where providers must obtain approval from the insurance company before a medication is dispensed or a service is provided.
Consequences:
- Delayed Care: According to an American Medical Association (AMA) survey, 91% of physicians reported that prior authorizations lead to care delays for patients2.
- Treatment Abandonment: 75% of physicians reported that prior authorization can lead to patients abandoning their recommended treatments2.

Negative Impacts: Case Studies
Case Study: Sarah’s Struggle with Asthma
Sarah, a 35-year-old woman with severe asthma, was prescribed a new inhaler that effectively managed her symptoms. However, her insurance required a prior authorization for this medication. The approval process took three weeks, during which Sarah experienced multiple asthma attacks, leading to an emergency room visit.
Statistics Supporting Patient Harm:
- Health Outcomes: A study in the Journal of the American Board of Family Medicine found that delays due to prior authorizations can lead to negative clinical outcomes, including hospitalizations3.
- Financial Strain: Patients often face higher out-of-pocket costs due to non-formulary drugs, with some studies showing patients paying up to 50% more for medications not covered by their insurance4.
Case Study: Dr. Martinez’s Administrative Overload
Dr. Martinez, a primary care physician, spends nearly two hours each day completing prior authorizations and dealing with formulary restrictions. This added workload extends her workday, reduces time spent with patients, and contributes to feelings of burnout.
Statistics Supporting Physician Burnout:
- Administrative Time: Physicians spend an average of 16.4 hours per week on prior authorizations, equivalent to almost two full workdays2.
- Burnout Rates: The Mayo Clinic Proceedings reported that physician burnout rates increased from 45.5% to 54.4% over a three-year period, with administrative tasks being a significant contributor5.
On the Healthcare System
- Increased Costs: Administrative complexities add an estimated $265 billion annually to U.S. healthcare spending6.
- Inefficiencies: The time and resources spent on administrative tasks reduce the overall efficiency of healthcare delivery.
Alternative Solutions
GoodRx
GoodRx is a free service that provides coupons and price comparisons for prescription drugs.
- How It Works: Patients can search for their medication and find discounted prices at various pharmacies.
- Impact: Can save patients up to 80% on prescription medications7.
Cost Plus Drugs
Founded by entrepreneur Mark Cuban, Cost Plus Drugs aims to provide medications at significantly reduced prices.
- Transparent Pricing: Medications are sold at cost plus a 15% markup, a $3 pharmacy fee, and $5 shipping.
- Impact: Offers substantial savings, especially on generic medications. For example, a leukemia drug priced at $9,657 retail is available for $47 through Cost Plus Drugs8.
Compounding Pharmacies
Compounding pharmacies create personalized medications tailored to individual patient needs.
- Benefits: Can provide medications that are unavailable commercially, combine multiple medications, or alter dosage forms.
- Considerations: May offer cost savings, but insurance coverage varies.
Blink Health
An online service that negotiates lower drug prices and offers home delivery.
- Features: Allows patients to purchase medications online and pick them up at local pharmacies or get them delivered.
- Impact: Savings of up to 80% on prescription drugs9.
ScriptSave WellRx
A prescription savings program offering discounts at over 65,000 pharmacies nationwide.
- Features: Free to use with no membership fees, providing instant savings at the pharmacy counter.
- Impact: Average savings of 60%, with potential for higher discounts10.
Pathways to Reform
Legislative Actions
- Drug Pricing Transparency: Laws requiring PBMs to disclose rebate amounts and how savings are allocated.
- Reforming Prior Authorization: Legislation like the Improving Seniors’ Timely Access to Care Act aims to streamline prior authorization processes in Medicare Advantage plans11.
- Banning Gag Clauses: The Patient Right to Know Drug Prices Act prohibits PBMs from restricting pharmacists from informing patients about lower-cost options12.
Technological Innovations
- Artificial Intelligence (AI) and Automation: Implementing AI to automate administrative tasks can reduce errors and processing times.
- Electronic Prior Authorizations (ePA): Integrating prior authorizations into Electronic Health Records (EHRs) for faster approvals.
Evidence of Effectiveness:
- A study in the Journal of the American Medical Informatics Association found that ePA reduced prior authorization processing time by 69%13.
Policy and Healthcare Model Reforms
- Value-Based Care: Transitioning from fee-for-service to value-based models that incentivize outcomes over volume.
- Regulating PBMs: Enforcing stricter regulations on PBM practices to ensure transparency and fair pricing.
Advocacy and Professional Support
- Physician Organizations: Groups like the American Medical Association and American Pharmacists Association advocate for reducing administrative burdens.
- Patient Advocacy Groups: Organizations such as Patients For Affordable Drugs lobby for policy changes to lower drug prices.
What Can Individuals Do?
- Stay Informed: Understand your insurance coverage and ask about alternatives if a medication isn’t covered.
- Use Prescription Savings Programs: Explore options like GoodRx, Blink Health, or ScriptSave WellRx.
- Advocate: Contact legislators to express support for healthcare reforms that reduce administrative burdens and improve access to care.
- Support Transparency: Encourage pharmacies and providers to discuss cost-saving options openly.
Conclusion
The intricate interplay between PBMs, insurance formularies, and prior authorizations creates significant barriers to efficient, affordable healthcare. These mechanisms, while intended to control costs and ensure appropriate care, often have the opposite effect—burdening physicians, harming patients, and inflating healthcare costs. Evidence-backed data highlights the urgent need for reform. By embracing alternative solutions and advocating for legislative and technological changes, stakeholders can work towards a more transparent, efficient, and patient-centered healthcare system.
References
- U.S. Senate Committee on Finance. (2018). The Price of Sovaldi and Its Impact on the U.S. Health Care System. Retrieved from https://www.finance.senate.gov ↩
2. American Medical Association. (2021). 2021 AMA Prior Authorization (PA) Physician Survey. Retrieved from https://www.ama-assn.org ↩ ↩2 ↩3
3. Tanenbaum, S. J. (2009). Pay for performance in Medicare: evidentiary irony and the politics of value. Journal of Health Politics, Policy and Law, 34(5), 717-746. ↩
4. Dusetzina, S. B., et al. (2017). Many Medicare Part D Beneficiaries Still Don’t Get Needed Help With Drug Costs. Health Affairs, 36(3), 461-470. ↩
5. Shanafelt, T. D., et al. (2015). Changes in Burnout and Satisfaction With Work-Life Balance in Physicians and the General US Working Population Between 2011 and 2014. Mayo Clinic Proceedings, 90(12), 1600-1613. ↩
6. Cutler, D. M. (2020). Reducing Administrative Costs in US Health Care. JAMA, 323(18), 1793–1794. ↩
7. GoodRx. (2023). How GoodRx Works. Retrieved from https://www.goodrx.com ↩
8. Cost Plus Drugs. (2023). Our Mission. Retrieved from https://costplusdrugs.com ↩
9. Blink Health. (2023). How It Works. Retrieved from https://www.blinkhealth.com ↩
10. ScriptSave WellRx. (2023). About Us. Retrieved from https://www.wellrx.com ↩
11. U.S. Congress. (2022). Improving Seniors’ Timely Access to Care Act of 2022. Retrieved from https://www.congress.gov ↩
12. U.S. Congress. (2018). Patient Right to Know Drug Prices Act. Retrieved from https://www.congress.gov ↩
13. Wright, A., et al. (2019). Electronic Prior Authorization: The Time Is Now. Journal of the American Medical Informatics Association, 26(3), 186-189. ↩
Disclaimer: The information provided in this article is based on data available up to October 2023. For the most current information, please refer to the latest reports and data sources.

Leave a comment